In mammals, the adrenal glands (also known as suprarenal glands) are endocrine glands that sit on top of the kidneys; in humans, the right suprarenal gland is triangular shaped while the left suprarenal gland is semilunar shaped. They are chiefly responsible for releasing hormones in conjunction with stress through the synthesis of corticosteroids such as cortisol and catecholamines, such as epinephrine. Adrenal glands affect kidney function through the secretion of aldosterone, a hormone involved in regulating plasma osmolarity.
Anatomy and function
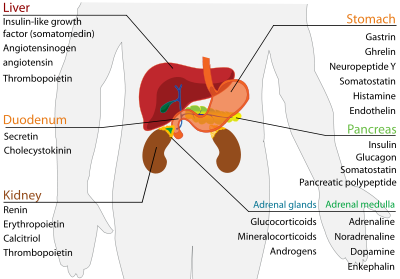
Anatomically, the adrenal glands are located in the retroperitoneum situated atop the kidneys, one on each side. They are surrounded by an adipose capsule and renal fascia. In humans, the adrenal glands are found at the level of the 12th thoracic vertebra. Each adrenal gland is separated into two distinct structures, the adrenal cortex and medulla, both of which produce hormones. The cortex mainly produces cortisol, aldosterone, and androgens, while the medulla chiefly produces epinephrine and norepinephrine. The combined weight of the adrenal glands in an adult human ranges from 7 to 10 grams.Cortex
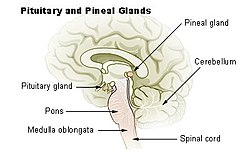
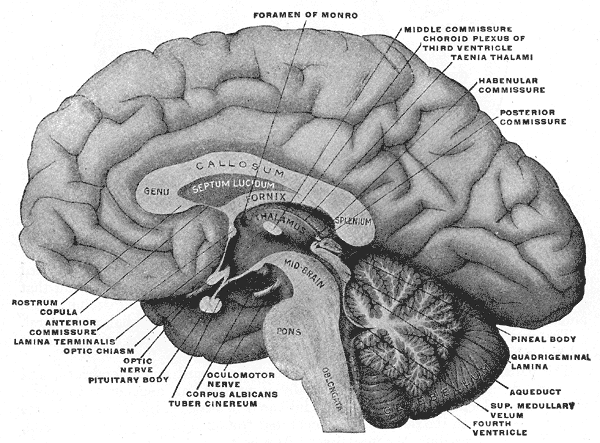
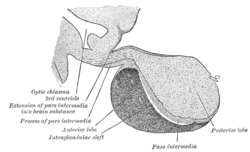
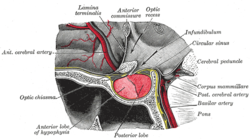
The adrenal cortex is devoted to the synthesis of corticosteroid hormones. Specific cortical cells produce particular hormones including cortisol, corticosterone, androgens such as testosterone, and aldosterone. Under normal unstressed conditions, the human adrenal glands produce the equivalent of 35–40 mg of cortisone acetate per day.[2] In contrast to the direct innervation of the medulla, the cortex is regulated by neuroendocrine hormones secreted by the pituitary gland and hypothalamus, as well as by the renin-angiotensin system.
The adrenal cortex comprises three zones, or layers. This anatomic zonation can be appreciated at the microscopic level, where each zone can be recognized and distinguished from one another based on structural and anatomic characteristics. The adrenal cortex exhibits functional zonation as well: by virtue of the characteristic enzymes present in each zone, the zones produce and secrete distinct hormones.
- Zona glomerulosa (outer)
- The outermost layer, the zona glomerulosa is the main site for production of mineralocorticoids, mainly aldosterone, which is largely responsible for the long-term regulation of blood pressure.
- Zona fasciculata
- Situated between the glomerulosa and reticularis, the zona fasciculata is responsible for producing glucocorticoids, chiefly cortisol in humans. The zona fasciculata secretes a basal level of cortisol but can also produce bursts of the hormone in response to adrenocorticotropic hormone (ACTH) from the anterior pituitary.
- Zona reticularis
- The inner most cortical layer, the zona reticularis produces androgens, mainly dehydroepiandrosterone (DHEA) and DHEA sulfate (DHEA-S) in humans.Medulla
The adrenal medulla is the core of the adrenal gland, and is surrounded by the adrenal cortex. The chromaffin cells of the medulla, named for their characteristic brown staining with chromic acid salts, are the body's main source of the circulating catecholamines adrenaline (epinephrine) and noradrenaline (norepinephrine). Derived from the amino acid tyrosine, these water-soluble hormones are major hormones underlying the fight-or-flight response.
To carry out its part of this response, the adrenal medulla receives input from the sympathetic nervous system through preganglionic fibers originating in the thoracic spinal cord from T5–T11.[4] Because it is innervated by preganglionic nerve fibers, the adrenal medulla can be considered as a specialized sympathetic ganglion.[4] Unlike other sympathetic ganglia, however, the adrenal medulla lacks distinct synapses and releases its secretions directly into the blood.
Cortisol also promotes epinephrin synthesis in the medulla. Produced in the cortex, cortisol reaches the adrenal medulla and at high levels, the hormone can promote the upregulation of phenylethanolamine N-methyltransferase (PNMT), thereby increasing epinephrine synthesis and secretion.
Blood supply
Although variations of the blood supply to the adrenal glands (and indeed the kidneys themselves) are common, there are usually three arteries that supply each adrenal gland:
- The superior suprarenal artery is provided by the inferior phrenic artery
- The middle suprarenal artery is provided by the abdominal aorta
- The inferior suprarenal artery is provided by the renal artery
Venous drainage of the adrenal glands is achieved via the suprarenal veins:
- The right suprarenal vein drains into the inferior vena cava
- The left suprarenal vein drains into the left renal vein or the left inferior phrenic vein.
The suprarenal veins may form anastomoses with the inferior phrenic veins.
The adrenal glands and the thyroid gland are the organs that have the greatest blood supply per gram of tissue. Up to 60 arterioles may enter each adrenal gland. This may be one of the reasons lung cancer commonly metastasizes to the adrenals.